Alzheimer’s is the most common cause of dementia in the UK, NHS notes. The exact cause of it is not fully understood, although medical professionals list potential factors that can lead to it, such as increasing age, untreated depression, a family history of the condition, and lifestyle factors and conditions related to cardiovascular diseases, among the rest.
However, in recent years, a growing number of scientific studies have backed up the belief that Alzheimer’s isn’t just a disease, but an infection.
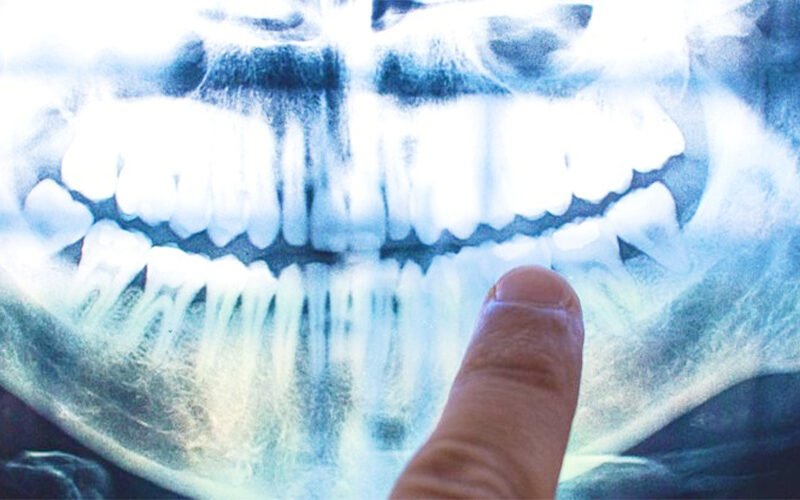
A 2019 study suggests that Alzheimer’s may be related to gum disease.
According to the research, led by senior author Jan Potempa, a microbiologist from the University of Louisville, the presence of Porphyromonas gingivalis – the pathogen behind chronic periodontitis (or gum disease) – was found in the brains of deceased Alzheimer’s patients.

A previous study by Cortexyme, Inc. found that mice orally infected with P. gingivalis produced higher levels of beta-amyloid (Aβ)—the sticky proteins commonly linked to Alzheimer’s disease.
“Infectious agents have been suggested as contributors to Alzheimer’s development before, but the evidence of causation has been unconvincing,” explained Dr. Stephen Dominy, Cortexyme’s co-founder.
Researchers also examined gingipains, the toxic enzymes of P. gingivalis, and found that high levels were associated with two other proteins already linked to Alzheimer’s: tau and ubiquitin.
However, they also detected these toxic gingipains in the brains of deceased individuals who had never been diagnosed with Alzheimer’s. This raises the question: Would these individuals have developed the disease if they had lived longer, or did Alzheimer’s itself contribute to poor oral health?

“Our discovery of gingipain antigens in the brains of individuals with Alzheimer’s—both those diagnosed with the disease and those with related pathology but no dementia—suggests that P. gingivalis infection in the brain is not merely a result of poor dental care after dementia onset or a late-stage consequence. Instead, it appears to be an early event that may explain pathology seen in middle-aged individuals before cognitive decline,” the researchers stated in their paper.
The mice study also showed that a compound developed by the company, COR388, reduced amyloid-beta production and neuroinflammation.
Whether this effect translates to humans remains to be studied.

“Drugs targeting the bacteria’s toxic proteins have so far only shown benefit in mice, yet with no new dementia treatments in over 15 years it’s important that we test as many approaches as possible to tackle diseases like Alzheimer’s,” chief scientific officer David Reynolds from Research commented.
Please SHARE this article with your family and friends on Facebook.